Society
Society


|
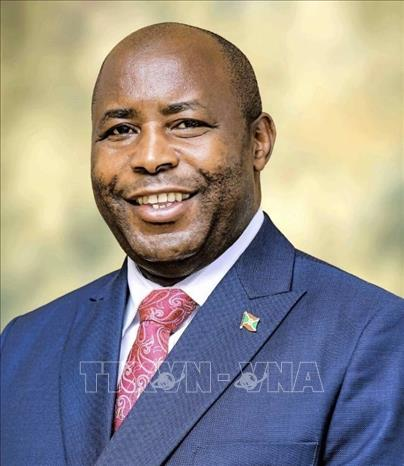
| Minister of Health Đào Hồng Lan. VNA/VNS Photo Thống Nhất |
Minister of Health Đào Hồng Lan speaks with Vietnam News Agency about a resolution on public healthcare issued on September 9, 2025 by the Communist Party of Việt Nam. Known as Resolution 72, it aims to reform the health sector and improve the well-being of all Vietnamese citizens. She also discusses the much-anticipated ‘free hospital fees’ policy and outlines the ministry’s bold new plans to strengthen healthcare services across the country.
The Party has issued Resolution 72, setting out breakthrough measures for the protection, care and improvement of public health. What significance does the resolution hold for the development of the health sector and public health in Việt Nam?
For decades, the protection and care of public health has received special attention from the Party and the State. Party congress documents, Central Committee resolutions as well as conclusions and directives from the Politburo and Secretariat have consistently set out clear orientations and priority objectives for safeguarding and improving the nation’s health. The role of healthcare has grown increasingly important within socio-economic policy. Nevertheless, the sector continues to face limitations, shortcomings and challenges.
Given pressing realities, healthcare services must undergo fundamental changes in thinking, awareness and practice. Over the past time, Party General Secretary Tô Lâm, Prime Minister Phạm Minh Chính and senior Party and State leaders have issued multiple directives on breakthrough solutions to strengthen healthcare services.
Resolution 72 reflects the Party’s deep concern for the well-being of every citizen, seeking to build a healthy Việt Nam where all people have access to quality healthcare, live longer and healthier lives, improve physical fitness, raise awareness of self-care and proactively prevent diseases. This contributes to the broader goal of a strong civilised and prosperous country in the new era.
Strategically comprehensive and long-term, the resolution is action-oriented, with new and strengthened policies to remove bottlenecks and obstacles, ensuring sustainable national development and meeting public expectations. It looks ahead to two historic milestones of the Party’s centenary in 2030 and the 100th anniversary of national independence in 2045.
A key feature of the resolution is shifting the focus from treatment to prevention, with primary healthcare and preventive medicine as the foundation, delivered at grassroots health stations. How will this be achieved?
The ministry will implement a series of breakthrough measures. Healthcare quality and effectiveness depend on three crucial factors: personnel, infrastructure and equipment, and financial mechanisms.
On human resources, primary healthcare and preventive medicine will be strengthened by allocating and mobilising staff, supported by preferential policies. Local health stations will be strengthened to ensure sufficient numbers of doctors and essential health workers, including village health staff and midwives.
From 2025 to 2030, at least 1,000 doctors per year will be seconded to commune-level health stations, with permanent staff gradually added. By 2027, each station will have four to five doctors; by 2030, staffing will meet official requirements. Training is a top priority, with dedicated schemes to produce doctors for remote, disadvantaged, border and island areas, and to develop high-quality training institutions at regional level.
On facilities and equipment, all commune health stations will be provided with the necessary infrastructure, medicines and basic equipment. The ministry will also ensure a stable and safe supply of vaccines, while promoting domestic vaccine production to meet the needs of the Expanded Immunisation Programme and prepare for emerging diseases.
Financially, commune-level health stations will operate as public service units providing essential healthcare, funded primarily by the State budget, with additional support mobilised from social resources. Public financing will focus on disadvantaged groups, remote and ethnic minority areas as well as specialised fields such as psychiatry, forensic medicine, emergency care and pathology.
The measures aim to realise the resolution’s spirit of 'innovation, acceleration and breakthrough', ensuring people receive comprehensive healthcare from prevention to treatment at grassroots level.
The 'free hospital fees' policy is attracting wide public attention. What will citizens actually benefit from, and how will fairness and efficiency be ensured?
By 2030, basic healthcare costs will be covered for all citizens through health insurance. This profoundly humane policy reflects the superiority of our political system, easing the financial burden on families, enabling early disease detection, and placing people at the centre of healthcare policy.
The ministry is urgently drafting an implementation plan. The policy will be phased in, with health insurance as its backbone. The State and insurance funds will cover essential medical costs, prioritising disadvantaged and low-income groups. Co-payment will be required for non-essential or high-demand services to promote individual responsibility and ensure cost-effective use of healthcare resources. Universal health insurance coverage will ensure risks are shared, with those better off supporting the less fortunate.
From 2026, citizens will be entitled to at least one free annual health check or screening, along with an electronic health record tracking their condition throughout life. By 2030, all basic medical costs within health insurance coverage will be free of charge.
The ultimate goal is equitable access to essential healthcare nationwide, reducing out-of-pocket payments and ensuring no one is left behind. This is not 'absolute free healthcare' but a major step towards reducing co-payments of citizens, expanding insurance coverage and building a fair, effective and sustainable healthcare system.
Resolution 72 also highlights healthcare personnel, medical ethics and special incentives for medical staff. How will the ministry attract, retain and empower its workforce?
Healthcare workers are the backbone of the system, dedicated professionals with skills and medical ethics. Investing in them is investing in development. The resolution introduces breakthrough measures in training, professional ethics and incentives.
First, on training, investment will go into high-quality medical schools, with tuition support and scholarships, especially for those committing to work in grassroots or disadvantaged areas.
Second, on incentives, special preferential policies will be applied to those working in preventive medicine and grassroots healthcare. Doctors and pharmacists will be ranked at higher salary grades, while frontline staff in remote and difficult areas will receive allowances of at least 70 per cent, rising to 100 per cent in the most disadvantaged regions. These incentives are designed to motivate and retain healthcare workers.
Third, on medical ethics and working conditions, professional standards will be revised and strengthened, with greater emphasis on training in medical ethics and communication skills. Working conditions will be improved to reduce stress and enhance job satisfaction, with management increasingly based on service quality and patient satisfaction.
How will the health sector turn the resolution’s objectives into reality?
The ministry will act with renewed determination in leadership, management and execution, ensuring rapid and effective implementation. Key steps include drafting and submitting new legislation, including laws on disease prevention, population, food safety, medical devices and traditional medicine; proposing Government decrees on training and allowances for healthcare workers; developing a national health action programme to guide ministries and provinces.
The ministry will roll out flagship projects, such as a national health and population programme (2026–35), pre-hospital emergency services, medical tourism, specialised health centres and free annual check-ups from 2026; accelerate digital transformation, including electronic health records and a national health database linked to population and insurance systems; strengthen public communication to raise awareness and mobilise citizen participation.
The resolution marks a timely and decisive step to remove bottlenecks, unlock resources and create breakthroughs in healthcare, covering institutions, financing, human resources, grassroots capacity and domestic production of medicines and equipment.
With strong Party and State leadership, coordinated action across the political system and society, and public consensus, Việt Nam’s health sector is positioned to build a healthier nation and contribute to a prosperous, civilised and sustainable future. VNS