 Society
Society

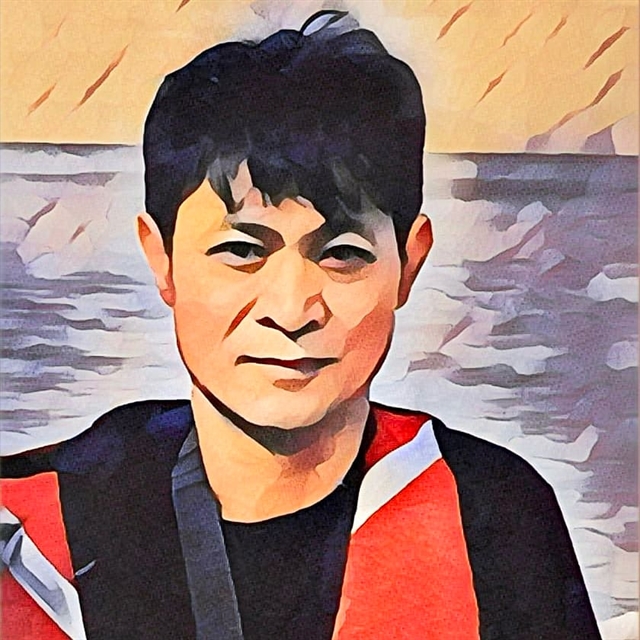 |
| Hồ Hồng Việt, a college lecturer-turned-writer. — Photo with AI app |
From this week, Việt Nam News presents sample chapters of the upcoming book in Vietnamese: Hồi ký chạy thận, Memoir of a Dialysis Patient, by Hồ Hồng Việt, who's entering his 19th year at the hospital. His first-hand accounts are both heart-wrenching yet encouraging for other patients in a similar condition. The book also reveals the hidden truth at some of the top hospitals in Hà Nội, where health workers could be found doing practices unfit for the job.
Việt Nam News hopes to receive your truthful comments if you're a reader, guidance or suggestion if you are a healthcare worker, or only a heart to encourage patients in similar circumstances. Please let us know on our fanpage. Follow the story on Việt Nam News website https://vietnamnews.vn/life-style
The Fateful Evening
One evening in early November 2006, I drove my wife to Dr. NLV's house, who works at BM Hospital, to ask him to look over my kidney function test results. He and his wife chatted with us for a while, then he picked up the test papers to examine them. I quietly observed.
At first, his expression was relatively calm. He reviewed the papers very carefully and I noticed he occasionally paused in thought, sometimes furrowing his brows. Naturally, I felt a bit anxious and worried. Finally, he set the papers down on the table and said:
- You have stage one chronic nephritis.
I felt a bit stunned but kept my composure and asked him:
- Can you explain it a bit more, doctor?
He didn't provide further details about my condition, just advised me to rest for a while and wrote me a prescription. I remember the prescription included the antibiotic Zinnat, with a dosage of three pills a day for five days, and I was told that I needed to undergo a specialist examination at the hospital. I understood that my condition was quite serious and I asked further: "Will my illness be treatable, doctor?"
The doctor replied: "The illness has progressed to a chronic stage and cannot be cured. You should be admitted to the hospital, and the doctors will run tests again and suggest a treatment plan."
My spouse and I said our goodbyes and headed home. The journey back was just over a kilometer, yet that evening it felt much longer; inexplicably, we both fell silent. At that moment, I wasn't preoccupied with my illness but rather felt a deep sense of affection for my wife. I wanted to ask her about things at home, but I didn't know how to start; I felt as if I had committed some grave error.
On the streets, traffic continued bustling, the lights along the road flickered through the flamboyant trees as they always did, and the welders were still busy, sparks flying like brilliant fireworks. Everything seemed unchanged, yet I felt a sense of alienation as if I were lost in a completely different world.
When I arrived home, my two children were still studying. They greeted us and then went right back to focusing on their work as if nothing had happened.
We have two children: our eldest is a girl, whom we affectionately call Tôm, and our second child is a boy, named Quick, who was born sixteen years after his sister.
That night, my wife and I lay awake, unable to sleep. By this point, we had both calmed down. My wife discussed what needed to be done in the coming days. I hardly dared to voice any opinions. Deep down, I felt it was best to follow my wife's suggestions (I agreed with whatever she said).
That evening could be seen as a fateful moment; I knew I was harboring a terminal illness, something I had never dared to think would affect me, and now I had to navigate the rest of my life alongside it.
CHAPTER I: BEFORE GOING ON DIALYSIS
BM Hospital
On the morning of November 3, 2006, my wife and I arrived at BM Hospital to meet Dr. NH, the Head of the Outpatient Department. As a friend, the doctor welcomed us warmly. He advised us to have Dr. KD, the Head of the Nephrology Department, treat me. However, Dr. KD was on a work trip to Japan and wouldn't return for another two weeks. I don’t know why at that time Dr. NH recommended that we go home, take medication to regulate blood pressure, and monitor it ourselves.
Seeing our hesitation, Dr. NH referred us to the Haematology Department, explaining that I was experiencing anemia and that treatment there might improve my kidney condition once my blood quality improved. The Head of Haematology, a female doctor, received us and admitted me for treatment. That was what I experienced in the early days at BM Hospital. Since I struggled to sleep, I requested outpatient treatment, with my wife driving me to the hospital in the mornings and picking me up in the afternoons. Each day, I received a blood transfusion and injections to stimulate red blood cell production (Eprex).
After about two weeks of this treatment, we asked to transfer to the Nephrology Department after hearing that Dr. KD had returned from his trip.
Holding the transfer document, I confidently approached Dr. KD, believing I would be admitted given my paperwork from the Hematology Department.
Initially, he firmly refused, citing the overcrowded condition of the department. Fortunately, I had also brought along the prescription written by Dr. NLV for him to review the lab results. After reviewing the document, Dr. KD changed his attitude and agreed to process my admission to the department.
My health was not good right now, and I had a lot of trouble sleeping, so my wife and I opted to stay in a service room, where each room had two beds, costing VNĐ350,000 per bed per day. The first treatment phase lasted about a month. During this time, my wife stayed in the hospital with me during the day, taking me to various functional examination rooms and managing my meals and medications. After taking care of everything, she headed home, usually around 9pm.
Every day, I received medication through an IV, had my blood pressure monitored, and got injections and various medications to maintain kidney function, fully following the doctor's orders. Perhaps the most striking moment during this treatment was one evening when my blood pressure rose, and I developed a severe headache. The doctor ordered a slow IV infusion of a low dose of Paracetamol. The infusion lasted from around 7pm until 4am when the pain finally subsided. Throughout that time, I writhed in pain. A headache from high blood pressure is incredibly uncomfortable and distressing; only those who have experienced this illness can fully understand the agony of such pain. I endured that pain for a solid eight hours. I expended all my energy to fight the pain and felt extremely fatigued; at times, I thought I might suffer a stroke. There were moments when I wished for that to happen just to end my prolonged suffering.
That night, I repeatedly sought advice from Dr. KD. By then, the doctor had gone home, telling me to wait until the infusion was complete. It wasn’t until 4am that the pain finally started to ease.
On that day, my wife didn’t dare go home and stayed awake with me all night. Even later, I still didn't understand why the doctor treated me this way. Before starting my treatment in the hospital, I was managing my hypertension myself. Besides taking medication regularly at scheduled times, whenever my blood pressure stayed high for an extended period and caused headaches, I would typically take additional medication to lower it. If necessary, I would also take more Paracetamol, which would quickly alleviate my headache.
That night at BM Hospital, I was only given a slow IV infusion of Paracetamol without taking any antihypertensive medication. According to the doctor, this method was to reduce the impact on my stomach and liver.
Since I was being treated in the hospital, I had to comply with the doctors' orders, but deep down, I found their explanation unconvincing. My liver was functioning normally, and my stomach was not in an acute inflammatory state; I had been taking blood pressure medication and Paracetamol for a long time. The headache that night was just an acute pain; with one dose of an antihypertensive and a pain reliever, it would have been resolved. It wasn’t a long-term treatment issue. If I had self-treated as I usually did at home, I believe I would have been headache-free within half an hour. That was the only time I treated my headache in that manner up to that point.
During this time, in addition to some standard medications, I often had to take some unfamiliar drugs that I hadn’t used before, like Corticosteroid (as I recall). When I asked, the doctor explained that it was related to the adrenal glands. Additionally, I had to take anti-inflammatory and immunosuppressive drugs like Medrol. I had to take these two medications daily at the hospital.
With my years of experience now, I am sure I would have researched the medication guides and effects thoroughly at that time. When I was discharged and went home, I was still prescribed those two medications, so I had to hire someone to come to my house to administer the injections. Noticing that I had to use these medications so frequently, I began researching the drug guidelines (I had to buy the medication myself, which included the instructions). During the treatment with these medications, I felt anxious and uneasy because I saw no positive changes in my condition, and my health continued to decline. I frequently felt very weak and exhausted.
After reading about the side effects of the medication, I was really worried but didn’t dare to stop taking it. There was another medication on the prescription; I vaguely remembered it was called Prednisolone, which served a purpose somewhat similar to Medrol. I took the medication for about two weeks. My spouse and I sensed a significant conflict between taking the medication and protecting the remaining kidney function.
Before being discharged, the doctor instructed me to have regular monthly check-ups for monitoring. I was scheduled for an appointment at a private clinic.
Personal reflections: Throughout my treatment in the hospital, the doctor communicated very little with us about the progression of the illness and was mostly treated in silence. When they did speak, it was primarily to inform us of the day's tasks, such as where to get imaging or ultrasounds done. Daily blood tests were taken, but we were unaware of what was being tested or the results. We only learned a little because my wife often went to the desk to check for any results related to my tests, and sometimes she got lucky.
Through these “sneak peeks,” we realised that my condition was unstable and had worsened. I only remembered that the creatinine level indicating kidney function at discharge was significantly higher than when I was first admitted.
Since the treating doctor didn’t discuss my medical condition with us, I naturally assumed I was still a first stage chronic kidney disease patient (whoever wants to think their illness is worse?). However, there was one detail I didn’t want to acknowledge: on the day I was preparing to be discharged, my spouse and I accidentally encountered Dr. ND, assistant to Dr. KD, in the hospital corridor. During a brief exchange of farewells, Dr. ND mentioned, possibly unintentionally, that my condition was transitioning from stage 1 to stage 2. I heard this but “brushed it off” and didn’t want to ask further, as the doctor conveyed the information in a way that suggested we should figure it out ourselves. In truth, I wasn’t surprised, as I had seen the test results and sensed my health was deteriorating.
Please read full story here.
Translated from Vietnamese by Nguyễn Huy Dũng




