 Society
Society

There are times when there’s bad news and even worse news. One such time is dealing with the problem of drug-resistant diseases in Việt Nam and elsewhere .
 |
| Illustrative image. Experts say some doctors added to the problem of antibiotics resistance by prescribing antibiotics unduly. — VNA/VNS Photo Hiền Hạnh |
by Thu Vân
HÀ NỘI – There are times when there’s bad news and even worse news.
One such time is dealing with the problem of drug-resistant diseases in Việt Nam and elsewhere .
Trung (not real name) was hospitalised a month ago after showing symptoms of pneumonia. After four days of treatment, however, his condition did not improve and he lost consciousness. Doctors at the National Hospital for Tropical Diseases in Hà Nội had to resort to endotracheal intubation (an emergency procedure) to keep him alive.
Susceptibility testing showed that he was resistant to all types of antibiotics except for colistin - a toxic antibiotic used to treat only the worst drug-resistant infections. After a month on endotracheal intubation, he regained consciousness and his condition has stabilised.
Thanh, 64, another patient who was taken to Vạn Hạnh Hospital in HCM City early last month, was not so lucky. Thanh resisted the strongest of antibiotics and was only sensitive to colistin and polymycin B. Three weeks after treatment, his condition worsened. His family took him home last week to await his demise.
Dr Dương Minh Tuấn said Thanh was the fifth such patient in a month that he’d seen, resistant to almost all types of antibiotics.
“We now have overwhelming evidence of rampant antibiotic resistance in most hospitals across the country, and it’s very worrying….” he paused, about to drop the bombshell.
“Because it means anyone of us can develop this resistance to antibiotics.”
“When one takes any type of antibiotics, naturally resistant bacteria will develop in his or her gut. These bacteria can be spread from him or her to anyone in contact, whether at home or in the community. If he is treated at a hospital, the bacteria can spread directly to other patients.
“Basically, it means that even if you don’t take antibiotics, when other people around you take antibiotics and develop resistant bacteria in their bodies, there’s a chance that you get those as well.”
This problem has been brewing worldwide for decades, but has not hit public consciousness in the country in a big way, although the World Health Organisation last year listed Việt Nam among countries with the highest antibiotic-resistant infections.
Nguyễn Vũ Trung, deputy director of the Central Tropical Diseases Hospital, said that the resistance rate to carbapenems, the strongest group of antibiotics, has risen to 50 per cent, mostly from gram-negative bacteria that have an impenetrable cell wall.
Resistance to third-generation cephalosporins, another powerful group of drugs, has surged to more than 60 per cent in the country, he said.
Recent individual studies have shown that Việt Nam has the highest prevalence of penicillin-resistance (71.4 per cent) and erythromycin resistance (92.1 per cent).
“This means that when treating a patient with antibiotics resistance, we will face many difficulties, including lesser choices of drugs, longer treatment time, higher costs, and sometimes, sadly, we can’t save the patients because no drug helps,” Trung said.
Two weeks ago, on September 21, the UN General Assembly held a high-level meeting to discuss how antibiotics have become less useful when treating human illnesses caused by bacteria. For the fourth time in its 70-year history, the UN elevated a health issue to crisis level, the previous occasions being HIV, the rise of non-communicable diseases such as heart disease, and Ebola.
The recognition by international agencies that antibiotic resistance is a global problem has come a bit late in the day, and it marks an acknowledgement that some of the miracles of modern medicine, including penicillin, could have run their course.
Antibiotics have been central to modern medicine, treating and preventing infections, protecting patients from pre and post surgical complication, the side-effects of cancer treatments, helping people with compromised immune systems, and treating and preventing diseases in livestock and other animals used as food.
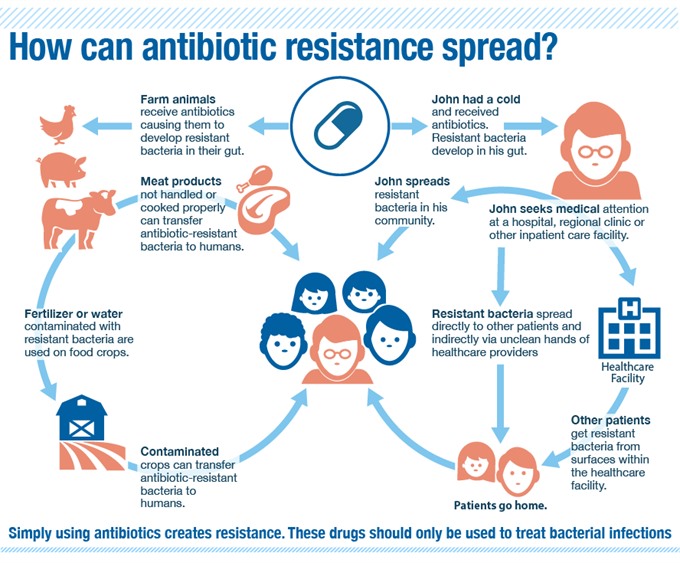 |
| This is how antibiotic resistance spreads. — Photo www.me-med.com |
However, widespread abuse of these drugs for many, many years now has borne fruit in a pandemic with horrifying implications.
Trung of the Central Tropical Diseases Hospital, who co-authored a 2013 report titled “Antibiotic use and resistance in emerging economies: a situation analysis for Việt Nam,” said overuse of antibiotics in human medicine as well as agriculture and livestock production was the main reason behind the growing problem.
The report, commissioned by Việt Nam’s Ministry of Health in collaboration with the Global Antibiotic Resistance Partnership and Oxford University Clinical Research Unit, studied 15 hospitals nationwide.
It said that in 2008-2009, antibiotics constituted an average 36 per cent of hospital treatment expenditure, and almost 40 per cent of this was accounted for by the third generation cephalosporin contributed a major part – 39.5 per cent. By value, the average antibiotic expenditure per hospital in 2008 was US$1.75 million. The highest spending on antibiotics ($6.74 million) was at the Chợ Rẫy Hospital in HCM City, followed by the Bạch Mai Hospital in Hà Nội, with $5.5 million.
Total drug sales in Việt Nam nearly tripled in value between 2001 and 2008, from $500 million to $1.4 billion. The report said no separate figures were available, but antibiotics were among the most widely used drugs.
The scary part is this: just 20 per cent of the country’s antibiotics use is from hospitals, and the rest happens outside, and most of this is “inappropriate,” according to doctors.
“Mothers often treat sick children without consulting a proper healthcare provider, and children with coughs and colds are given antibiotics,” Trung said.
A 2007 study had found that general knowledge on antibiotics was poor among the community. Self-treatment was common, as was incorrect dosage or duration. To this day, antibiotics can be purchased over the counter at pharmacies without the legally-required prescription. Trung said some doctors added to the problem by prescribing antibiotics unduly.
The 2013 report said that in rural and urban pharmacies in the country, 88 to 91 per cent of all antibiotic sales (sample taken in 2010) were without prescription. A pharmacist in Hà Nội who insisted on anonymity said while he was aware of the law, he had to keep his customers.
"First, I can’t compete with other drug stores if I ask for a prescription. Secondly, if I don’t give them antibiotics and their illness symptoms don’t go away, they would not return the next time."
Even less reassuring was a 2009 study’s finding that just 27 per cent of pharmacy staff had correct knowledge of antibiotic use and resistance.
Cao Hưng Thái, deputy director of the Examination and Treatment Department under the Ministry of Health, blamed the abuse of antibiotics on lax management of antibiotics and mild penalties.
“People keep joking that they can buy antibiotics as easily as buying vegetables,” he said.
“While we do have adequate regulations on the sale of antibiotics, according to which certain types of antibiotics can only be purchased with prescription, it’s obvious that enforcement is not effective," he said.
Thái said a motely inspection force with the health ministry has to oversee more than 30,000 healthcare institutions and more than 30,000 drugstores and pharmacies in the country. Furthermore, most clinics and hospitals lack the equipment and human resources to carry out susceptibility tests and determine which type of antibiotic can be administered to a patient.
“At the grassroots level, doctors often prescribe antibiotics based on their experience, which is also limited. This also leads to inappropriate use of antibiotics," Thái said.
 |
| Experts say overuse of antibiotics leads to more antibiotic-resistant infections. — VNA/AFP Photo |
Significant amounts of antibiotics used by people and animals eventually find their way into the environment, particularly in surface and ground water and in the soil. Antibiotics-resistant bacteria arise and spread in animals and in the environment, and, sometimes, to humans through several ways.
In Việt Nam, the use of antibiotics in livestock breeding has been increasing over the last several decades.
The 2013 study estimated that 70 per cent of pharmaceuticals used in animals are antibiotics. Many antibiotics used to treat human diseases are used in agriculture and farmers often do not comply with regulations requiring them to stop the use of these drugs before harvesting their products.
Dr. Soccoro Escalante, Health System Development Coordinator of the WHO, confirmed this.
“In the animal sector, inappropriate use of antibiotics in animal husbandry and aquaculture drive antimicrobial resistance. This will in effect have dangerous impacts on human health, through the transmission of antimicrobial resistant organisms and the existence of antibiotic residues in the food chain,” she said.
Environmental contamination is also a big factor as resistant bacteria from human and animal waste can be spreaded out via unsafe waste disposal from hospitals and poor sewerage systems add to the problem. Antibiotic residues in water and soil can also compound the emergence of resistant bacteria in the environment.
The ministry launched in 2013 an action plan to deal with antibiotics resistance.
The plan called on hospitals to improve consultancy on medicines as well as management of infections. It introduced stricter regulations on the use of antibiotics and advanced equipment.
Since then, “doctors and pharmacists have become better aware of the importance of proper use of antibiotics as well as the seriousness of antibiotics resistance," said Trung from the National Hospital for Tropical Diseases.
In June 2015, WHO supported the Government in convening a high level inter-sectoral meeting, during which an Aide Memoire for Multi-sectoral Action to Combat AMR was signed.
“WHO strongly recommends that Việt Nam pursue this high-level multi-sectoral commitment, ensuring that policies and regulations at the national level are strong, while at the same time, advocating and monitoring for local actions at all levels, at the provinces, districts and communities,” Soccoro said.--VNS
Elephants in the roomAmidst all the analysis of antimicrobial resistance, some fundamental causes are rarely mentioned or highlighted, and these elephants in the room could well end up trampling all efforts to deal with the problem. Poverty has been cited by the WHO itself as a major force driving antimicrobial resistance. In developing countries, inadequate access to effective drugs worsens unregulated dispensing and manufacture of antimicrobials, and “truncated antimicrobial therapy because of cost are contributing to the development of multidrug-resistant organisms." In 2007 a study by Dr Margaret Planta noted this: "Poverty-stricken patients may forgo the cost of a physician consultation and self-medicate. They may be more likely to purchase the least expensive (and possibly least potent drug) under the assumption that they are all bioequivalent. Furthermore, these people may only complete a truncated course of therapy because of their inability to pay for the full course of medications." | ||||||
Dr Soccoro Escalante, Health System Development Coordinator, WHO Antimicrobial resistance is a complex and multidimensional issue. It is therefore important for the Government and the public to be vigilant and to take every single action needed to fight it. We have strong evidence, via the monitoring undertaken in hospitals and in the agricultural sector, about the existence of a number of resistant bacteria in Việt Nam that are very dangerous to human health.
Cao Hưng Thái, Deputy Director of the Examination and Treatment Department under the Ministry of HealthThe practice of healthcare providers prescribing antibiotics is still troublesome. Some doctors prescribe antibiotics, or a more expensive kind of antibiotic, which may not be truly necessary -- antibiotics which may have limited benefit. Meanwhile, in the agriculture and livestock sectors, we don’t have an adequate legal foundation to regulate the use of antibiotics. I think we need better co-operation between the health sector and the agriculture sector to monitor, and eventually ban the use of certain types of antibiotics.
Nguyễn Thị Kim Tiến, Minister of HealthSelf-medication happens because people do not want to go to hospitals because our primary healthcare system has not been able to cover everyone. |




