 Society
Society

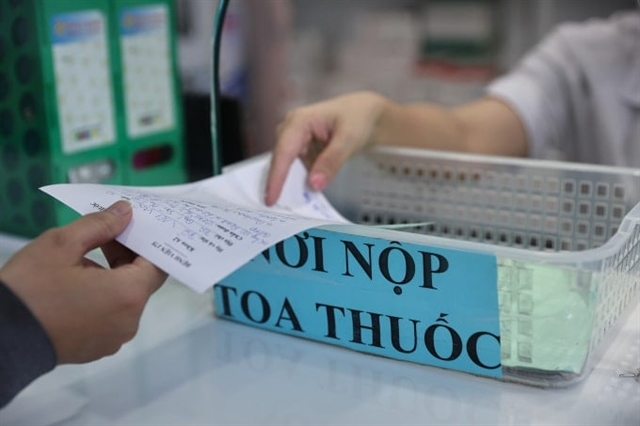 |
| Medical staff at the pharmacy of Military Hospital 175 in HCM City dispense medication to patients. — VNA/VNS Photo |
HCM CITY — The Ministry of Health has issued a final deadline requiring all hospitals nationwide to implement electronic prescriptions (e-prescriptions) by Oct 1, marking the third extension of the mandate due to prolonged delays.
The requirement is part of a new circular regulating prescriptions and the use of chemical drugs and biologicals in outpatient treatment, which took effect July 1.
Under the circular, hospitals must fully adopt e-prescribing systems by Oct 1, and other healthcare facilities, including clinics and private practices, by Jan 1, 2026.
This is the third time the ministry has extended the timeline. The previous deadline, under Circular No. 04/2022, required facilities to connect their prescription data to the national system by June 30, 2023.
Electronic prescriptions are considered a key component of the broader electronic medical record system and are required even for outpatient visits that do not involve complete medical records.
Nationwide adoption is seen as essential for monitoring and managing prescription and drug dispensing practices throughout the healthcare system.
National e-prescription platform
The Ministry of Health has already launched a national e-prescription management platform, featuring a centralised database with hospital IDs, doctor IDs, and prescription codes.
The system is designed to handle up to 600 million prescriptions per year.
Speaking at a recent conference, Nguyễn Hữu Trọng, general secretary of the Vietnam Health Informatics Association, said the platform aimed to connect all public and private prescriptions through unique identifiers, allowing pharmacies to securely verify and dispense medication.
“The goal is to prevent the use of outdated or unauthorised prescriptions, reduce medication errors, and phase out handwritten or unverifiable prescriptions,” he said.
Trọng warned that the current paper-based system lacked transparency, making it difficult to confirm the accuracy or legitimacy of prescriptions, which contributed to widespread drug misuse and public health risks.
Despite the system’s capabilities, implementation remains slow. Only about 12,000 of more than 60,000 medical facilities nationwide are currently connected, according to Trọng.
Many major hospitals have only adopted e-prescriptions for insured patients, leaving out those who pay out of pocket.
Private clinics lag even further, with an estimated 40,000 facilities yet to link their systems.
On the pharmacy side, just 3.6 million out of 218 million e-prescriptions have been confirmed as dispensed, underscoring a major compliance gap.
Many hospitals still rely on paper prescriptions or outdated software that fails to meet national standards or connect to the central database. Even some hospital pharmacies do not verify prescriptions using electronic codes.
Trọng said technical barriers were minimal, as most healthcare software could integrate with the system without affecting doctors’ workflows.
Retail pharmacies also stood to gain from more efficient operations and reduced manual input.
However, he pointed to insufficient training, inspections, and enforcement as major issues. “No healthcare provider has been penalised so far, even though penalties are clearly outlined in existing regulations,” he said.
Resistance to transparency and fear of oversight remained major obstacles, especially in the private sector. “Many providers fear being monitored or penalised for overprescribing or unauthorized drug sales,” he added.
Trọng called on the government to ramp up enforcement, educate the public on the need for prescription-based drug purchases, and impose stricter penalties to ensure full compliance nationwide. — VNS




