Life & Style
Life & Style

|
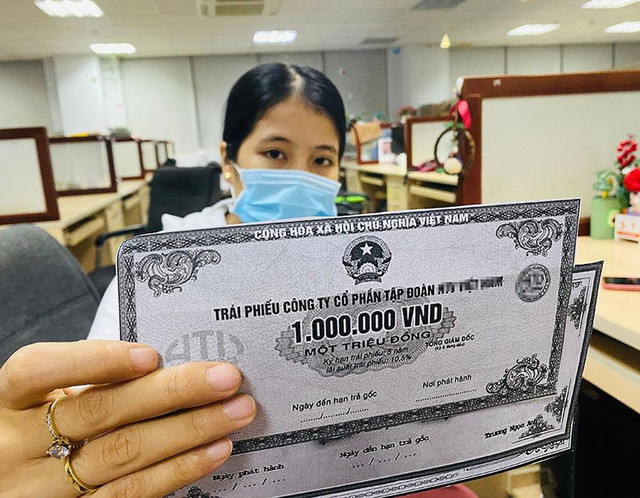
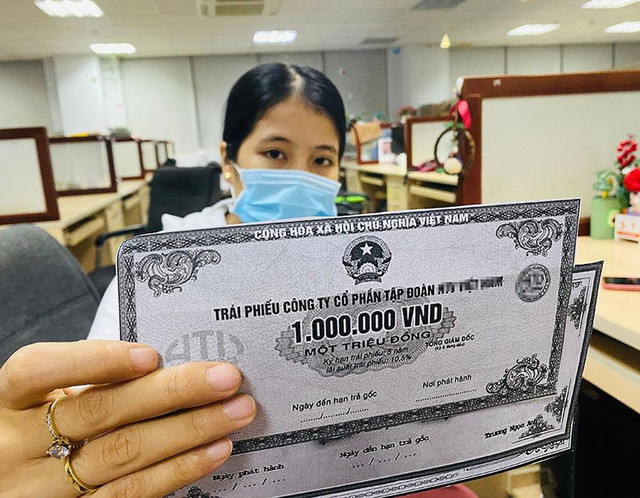
| Intensive Care Unit in Italy during Covid-19 pandemic. Photo courtesy of Family Medical Practice |
Nearly 17,000 people have died of Covid-19 infection in Italy in just two months. The high death rate has caused concern globally. Italy has a high average age which may be one of the causes. But that is not the whole explanation. Italy's underlying antibiotic resistance crisis has probably worsened the situation dramatically.
A deadly mix of coronavirus and multi-resistant bacteria may be the cause of high death rates in Italy. Many people who are infected with Covid-19 in Italy probably don’t die from the virus itself, but coupled with a vigorous immune response, the so called “Cytokine storm”, and very importantly from secondary infections caused by bacteria resistant to almost all antibiotics or “superbugs”.
Italy is the country in Europe where most people die from resistant bacteria, nearly 11,000 each year. Data from the European Centre for Disease Control (ECDC) in Stockholm shows that superbugs are now endemic in Italian hospitals, causing 30 per cent of all bacterial infections. If a Covid-19 patient gets a secondary bacterial infection at an Italian hospital, it is therefore very likely that it is a “superbug” and cannot be treated.
During the 2009 H1N1 epidemic 300,000 lives were lost, it is estimated that up to about half of deaths were caused by secondary bacterial pneumonia. Secondary bacterial infections also to play a crucial role in Covid-19 mortality. Over half of patients who died from Covid-19 had a secondary bacterial infection in Wuhan, China, according to a study recently published in the Lancet.
Viral respiratory infections generally weaken the immune system, allowing bacteria to attack more easily. Covid-19 differs from regular seasonal influenza in that about 20 per cent of the patients develop viral pneumonia and need in-hospital treatment and oxygen. About five per cent develop serious pneumonia and need mechanical ventilation, and in exceptional cases, if the lungs are unable to supply enough oxygen to the blood, ECMO treatment might be needed.
Antibiotics have no known effect on the SARS-CoV-2 virus, but to prevent secondary bacterial infection, antibiotics are often administered to more severe cases. Even with aggressive, virus-based pneumonia, it is usually possible to recover. If the bacteria are susceptible antibiotics can treat or prevent secondary bacterial infections allowing the immune system to concentrate on fighting the viral infection. This might be one reason for the much lower mortality rate in Germany, having lower prevalence of superbugs in their hospitals.
Việt Nam’s response to the Covid-19 epidemic is very successful. In the first phase with the epidemic in Hubei, China, the Vietnamese authorities, healthcare system and civil society was rapidly mobilised. The border to China was closed, all people coming from epidemic areas were quarantined for two weeks, contact tracing implemented, if symptomatic Covid-19 test was performed. The initial 16 Covid-19 cases all recovered.
Now with the pandemic in 'full swing', people with Covid-19 infection might come from any country. Hence all borders have closed since last week. At the time of writing there are over 240 diagnosed Covid-19 cases in Việt Nam, no deaths and no verified community transmission (where persons with no clear path of transmission have been detected in community). However, the cases in Bạch Mai hospital, now in quarantine, might indicate the initiation of community transmission.
In comparison to Italy the population of Việt Nam is larger, 100 million compared to 60 million. Việt Nam has a much younger average age, which might decrease the severity of an outbreak. However, most households have several generations which make it more difficult to protect the elderly, who are more venerable. In addition, the proportion of healthcare personnel and hospital beds per capita in the Vietnamese healthcare system is much less, central hospitals normally are over-crowded resulting in patients often having to share beds. Considering the consequences of a generalised Covid-19 epidemic the forceful preventive measures taken by the Vietnamese authorities are crucial.
In the unfortunate event of a generalised Covid-19 epidemic in Việt Nam the deadly mix of Covid-19 and superbugs might be even more severe than in Italy considering the high rates of antibiotic resistant bacteria causing Hospital Acquired Infections (HAI). Studies in hospitals throughout Việt Nam showed that half of all patients are colonised with superbugs resistant to most available antibiotics. In Intensive Care Units one third of the patients had HAI commonly with superbugs, resulting in longer treatment times, higher costs and mortality.
What can be done to prevent this deadly mix of Covid-19 and superbugs? The most important is what is currently done – to proactively prevent community spread of Covid-19 with the promotion of good hand hygiene, early detection of cases, isolation, and contact tracing as well as social distancing.
And what about prevention of superbugs? Amazingly it is the same measures needed to decrease superbug colonisation and HAI that now Việt Nam has shown to be outstanding in implementing at society level – good hand hygiene, early detection of cases though testing using bacterial cultures and isolation to prevent transmission. In a study where all patients at three Vietnamese pediatric intensive care units were screened at admission for superbugs and isolated if positive, the transmission of superbugs was reduced to almost half.
If the proactive measures taken to prevent a Covid-19 epidemic are successful – a national intervention to prevent superbugs and HAI will still save many lives and enormous recourses – in the unfortunate event of Covid-19 epidemic in Việt Nam even more loved ones could be saved by decreasing the deadly Covid-19/superbug mix – hence a win-win strategy. – Family Medical Practice.
Authors:
Mattias Larsson, MD, PhD, Associate Professor, Family Medical Practice Hanoi, Department of Global Public Health, Karolinska Institutet, Stockholm, Honorary Professor, Hanoi Medical University
William Brian McNaull, MD, MPhil (Cantab), DTM&H ( London), Medical Director, Family Medical Practice, Hanoi
For more advice on any medical topics, visit Family Medical Practice Hanoi at: 298 I Kim Mã, Ba Đình. Tel: (024) 3843 0748. E: hanoi@vietnammedicalpractice.com.
FMP’s downtown Hồ Chí Minh location is: Diamond Plaza, 34 Lê Duẩn, District 1; 95 Thảo Điền Street, District 2. Tel: (028) 38227848. E: hcmc@vietnammedicalpractice.com
FMP Đà Nẵng is located at 96-98 Nguyễn Văn Linh Street, Hải Châu District, Đà Nẵng. Tel: (0236) 3582 699. E: danang@vietnammedicalpractice.com.