Society
Society

 |
| Quinten Lataire, acting country director for UNAIDS in Việt Nam. Photo courtesy of UNAIDS |
Quinten Lataire, acting country director for UNAIDS in Việt Nam, talks to Việt Nam News reporter Nhật Hồng on the country’s HIV response on the sidelines of the second Southeast Asia Regional Workshop on HIV-related stigma and discrimination held early this month in Bangkok, Thailand
What is the current progress in addressing HIV/AIDS in the region and particularly in Việt Nam?
Asia and the Pacific has seen an overall decline in new HIV infections since its peak at the end of the last century, but that decline has significantly slowed down in the last decade and some countries within the region have even seen a substantial increase in new HIV infections, such as the Philippines. The HIV epidemic in the region also disproportionately affects people from key populations, especially young people. In the Philippines, for instance, new infections among men who have sex with men (MSM) have seen a six-fold increase, while in Laos new infections among MSM doubled and in Cambodia that number has tripled since 2010.
In Việt Nam, while there has been a commendable decline in new HIV infections overall, there is a concerning trend of rising infections among MSM since 2010. A significant proportion of these new infections, one third, occurs in young people between 15 and 24 years old. This highlights a concentrated epidemic within Việt Nam where MSM are disproportionately affected, and within the MSM group, you see that young people are specifically vulnerable to HIV.
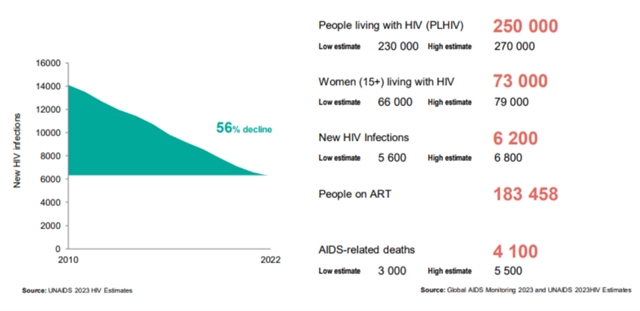 |
| Snapshot of Việt Nam's HIV/AIDS data, released by the UNAIDS in 2023. VNS Screenshot |
What is the current situation regarding stigma/discrimination towards people living with HIV (PLHIV) in the region? Could you share some of the best practices in the region and the recommendations for Việt Nam?
Let me first explain the difference between stigma and discrimination. HIV-related stigma refers to the negative beliefs, feelings and attitudes towards PLHIV as well as groups associated with PLHIV, such as the families of PLHIV, and other key populations at higher risk of HIV infection, such as people who use drugs, sex workers, men who have sex with men, transgender people and people in detention. HIV-related discrimination, on the other hand, refers to the unfair and unjust treatment of an individual based on his or her real or perceived HIV status.
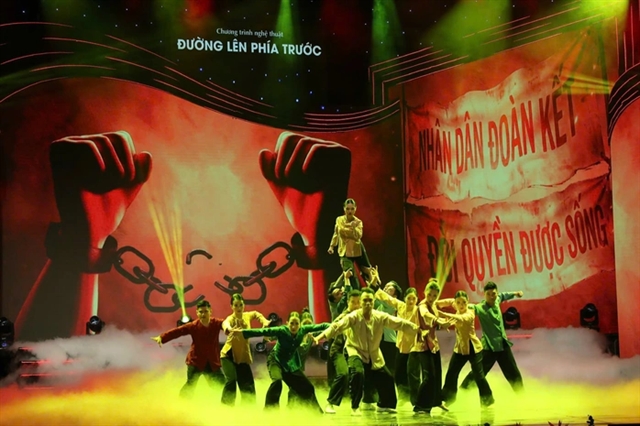
There is a whole body of evidence when it comes to stigma and discrimination reduction programming. Community organisations in Việt Nam have been very active in implementing specific intervention models. One example is the PLHIV Stigma Index which, in Việt Nam, is being implemented by the Vietnam Network of People Living with HIV (VNP+). The Stigma Index is a standardised tool to gather evidence from PLHIV on how stigma and discrimination impact their lives. That community-led data collection is an important stigma measuring tool for effective programming.
Another example is the mobilisation of key opinion leaders and mass media to reduce HIV-related stigma and discrimination that the Blue Sky Social Enterprise has been engaging in. They have been leveraging the power of key opinion leaders, such as journalists, artists, beauty pageant winners and more broadly the mass media, to strengthen public HIV awareness raising and call for the reduction of HIV-related stigma and discrimination.
The number of PLHIV among the MSM group is seeing an upward trend. How do you evaluate Việt Nam’s action plans and measures regarding this trend? What should be done to intervene and curb the rise of infections among this group?
Let me first highlight the fact that Việt Nam, in its HIV response, has been very successful. Việt Nam stands out as one of the leading examples in this region when it comes to an effective HIV response. This success is the result of the work of Việt Nam’s strong national HIV authority, complemented by substantial support from international partners. These collaborative efforts have resulted in a strong overall decline in new HIV infections in Việt Nam.
For example, in response to the rising epidemic among people who inject drugs two decades ago, Việt Nam implemented effective evidence-based interventions such as needle and syringe programmes and methadone, and that has proven to be highly effective. This health-centred approach has led to a notable decline in new infections among people who inject drugs and their communities.
The landscape of the epidemic is shifting, with a concerning rise in new HIV infections among young MSM. That also requires programmatic adjustments. Young MSM, for instance, need to have more access to prevention measures such as PrEP (pre-exposure prophylaxis). PrEP is a cost-effective measure to reduce the HIV epidemic among that specific group of people and an important tool to get the epidemic in the country going down.
 |
| A community-based organisation in the northern province of Thái Nguyên consults with a client on HIV prevention and control measures. VNA/VNS Photo Dương Ngọc |
What are the roles of community-based organisations (CBOs) and private healthcare facilities in HIV/AIDS prevention and control in Việt Nam?
CBOs and private healthcare facilities have a very important role to play. You can see them as the extended arm of the public health system. CBOs and private healthcare facilities can help address potential gaps in the HIV response. For example, some people might not be able to visit public health facilities during opening hours or would like to get peer counselling. Private health clinics and CBOs can have different opening hours, or they can provide online peer support from a person living with HIV or from someone from a key population group. As such, they make sure that we leave no one behind in the HIV response.
Sustainable financing is crucial for the long-term success of HIV/AIDS programmes. How is UNAIDS advocating for increased investment in HIV response efforts in the region and Việt Nam?
Different countries are at various stages of their HIV response. Việt Nam has proven to be overall very successful.
On a global scale – and I need to stress that this has nothing to do with Việt Nam’s performance – there is a concerning trend of declining funding for HIV. In light of this situation, there is a growing need for greater domestic resources in Việt Nam, particularly for prevention efforts. These financial resources should be allocated both nationally and at the provincial level, aligning with the decentralisation of Việt Nam’s healthcare system. Ensuring sufficient domestic funding at the provincial level is essential to guarantee comprehensive coverage of all prevention and treatment measures across the country.
What can Việt Nam do to reduce stigma and discrimination compared to other countries that might be more open in terms of gender diversity?
Comparing countries can be challenging because of different systems and political dynamics. However, one observation stands out: when legal and policy environments are supportive of key population groups, stigma and discrimination decrease, leading to fewer barriers. This, in turn, reduces new HIV infections, resulting in a more effective HIV response.
It's very simple: if you criminalise people for who they are, they will go underground. If people go underground, it will be much harder for them to get access to healthcare. So, these things are very much correlated. Again, the more enabling the legal and policy environment, the more effective your HIV response will be.
In addressing stigma and discrimination, it is crucial to target the specific causes driving them. For example, if a healthcare worker wears two pairs of gloves when treating someone with HIV, it is an irrational response stemming from fear or ignorance. To combat this, efforts should focus on dispelling these fears and ignorance. Effective stigma reduction programmes directly tackle these underlying drivers of stigma.
So addressing the underlying drivers of stigma will also create a more effective policy and legal environment. If you have a more effective policy and legal environment, you will have a more effective HIV response. It is all very much interrelated. VNS
*This interview has been edited for length and clarity.