.jpg) Society
Society

Eight years ago, Nguyễn Thị Lành (not her real name) of HCM City was diagnosed with hepatitis B, and several months later, she became pregnant.
 |
| The World Health Organisation recommends that all infants receive a hepatitis B vaccine as soon as possible after birth, preferably within the first 24 hours. Source tiemchungmorong.vn |
Gia Lộc
HCM CITY — Eight years ago, Nguyễn Thị Lành (not her real name) of HCM City was diagnosed with hepatitis B, and several months later, she became pregnant.
Armed with the knowledge that she had tested positive for hepatitis, she told her doctors, who, within 12 hours after delivering her baby, provided hepatitis B immunoglobulin and a hepatitis B vaccine to the newborn.
Following medical protocols established by the Việt Nam National Expanded Program on Immunization, the doctors also gave the baby three doses of a hepatitis B vaccine.
Afterwards, the baby tested negative for hepatitis B surface antigens (HBsAg), the first serologic marker to appear in a new acute infection.
The test also showed that hepatitis B surface antibodies (anti-HBs) were more than 1,000 international units per litre, showing that the child had not contracted hepatitis.
When anti-HBs levels of children are under 1,000 international units per litre after three vaccine doses, and their infected parents and relatives live in the same house, the children must be vaccinated again.
Unlike Lành, a woman from a south-central province who gave birth eight years ago to a son, was not so lucky.
Because the woman had not received counselling at her local hospital about hepatitis B, she had not received intervention to prevent hepatitis B virus (HBV) transmission at that time.
After finding out that she had hepatitis two months ago, the mother took her son, now eight years old, to the HCM City Hospital for Tropical Diseases for tests, which showed that he had contracted the hepatitis B virus.
As tests indicated that the child had a low viral load and an uninflamed liver, the child and the mother are now being monitored every six months with blood tests, and are expected to recover.
Babies and young children infected with hepatitis B are more likely to have a chronic condition.
Ninety per cent of newborns develop chronic hepatitis B infections after six months if no perinatal (a number of weeks immediately before and after birth) intervention is provided, according to Dr Tô Ngọc Nga of HCM City University of Medicine and Pharmacy, who spoke at a conference in July about elimination of viral hepatitis B and C in Việt Nam held in HCM City.
Dr Trương Hữu Khanh, head of the city’s Paediatrics Hospital 1’s infectious and nervous diseases department, said that he had seen several fatalities related to hepatitis B.
“The disease can lead to acute liver failure in children or even a coma. Treatment for children is more difficult than for adults because of the shortage of appropriate drugs,” Khanh said.
Around 10-12 per cent of the country’s pregnant women in 2014 contracted chronic hepatitis B, according to the Ministry of Health’s statistics issued in 2015.
Two per cent of children aged under 5 in the country were infected with hepatitis B in 2014, the latest figures available, according to the ministry.
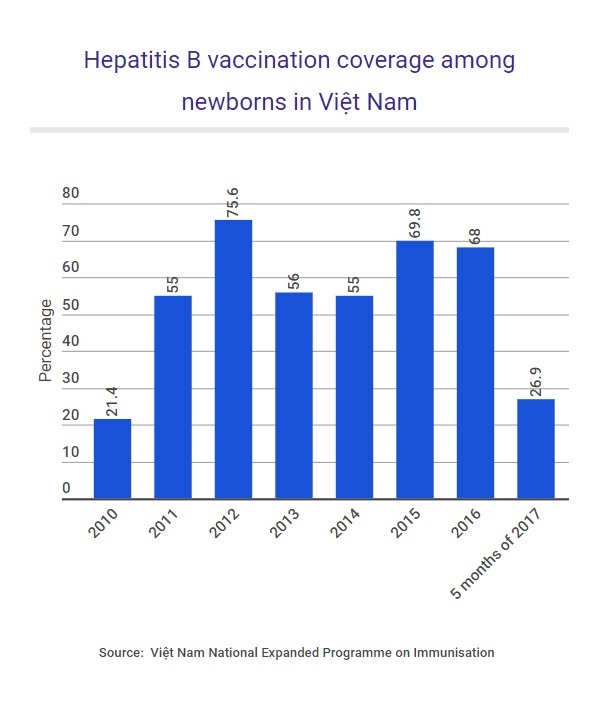 |
| VNS Infographic Thu Hà |
Prevention
“Chronic infections are preventable if women have blood tests to detect HBV infection before pregnancy,” Khanh said.
If they test positive for HBV, the mother must visit specialised hospitals for treatment and their infants must receive hepatitis B immunoglobulin and vaccine as soon as possible after birth, he added.
These infants should get three doses of hepatitis B vaccine during the first year of life, he said.
With such treatment, the effective rate of prevention of perinatal HBV transmission is more than 95 per cent, he said.
“Several hospitals in the country, especially in rural areas, still do not have hepatitis B immunoglobulin for intervention,” leading to a risk of mother-to-child transmission, Khanh said.
For the first five months of this year, the vaccination rate against hepatitis B among newborns in the country was 26.9 per cent, while 68 per cent were vaccinated last year, although the vaccine has been available since 1982, according to a report from the Việt Nam National Expanded Program on Immunization.
Dr Nga of the HCM City University of Medicine and Pharmacy said that vaccination was an effective prevention.
“An education programme on the importance of the vaccine should be provided to people, especially to women aged 15 to 49,” she added.
Dr Đặng Lê Dung Hạnh of Hùng Vương Hospital said that few women had received the vaccine against HBV before pregnancy.
Many women aged 15 to 49, especially in rural areas, do not receive counselling or tests, even those under a doctor’s care.
Hạnh said that national guidelines on reproductive health care services issued last year by the Ministry of Health did not include warnings about the need for vaccinations.
Khanh of the Paediatrics Hospital 1 said that if vaccination among infants was widespread, the country’s goal by 2017 of having less than 1 per cent of children aged under five infected with HBV could be reached.
Other health experts suggested that links between obstetrics and paediatrics hospitals should be strengthened to improve intervention and treatment.
Obstetrics hospitals should also have counselling rooms for pregnant women, they added.
Việt Nam is among the countries suffering the most from viral hepatitis B and C, with a disease prevalence of 10 to 20 per cent of the total population, according to Dr Trương Thị Xuân Liễu, chairwoman of the HCM City Medical Association.
Liver cancer is ranked third in the number of all cancer cases in the country, she said, added that all resources from the health sector as well as the community should be exploited to deal with the situation. — VNS









.jpg)